[ad_1]
Are narrow networks a good thing or a bad thing? The first thing you need to know is what a “narrow network” is. Narrow network is an informal term that basically means that your health plan either imposes restrictions on the providers you can see and/or you have higher cost-sharing levels for some providers outside of the network .
On the one hand, a narrow network can be a good thing. If provider network limitations make it more difficult to see low-quality or high-cost providers, this could lead to lower premiums with no impact on patient care. However, if these provider network limitations limit choice and quality is difficult to measure, patients may be made worse by a narrow network.
A sort of RWJF Issue Brief by Corlette et al. (2022) Aims to define what will constitute and an appropriate network. The following table shows a common hierarchy.
There are four main criteria for measuring network adequacy:
- time and distance. Determine the maximum travel time (measured in miles or travel time) to visit a given provider.
- Provider to Enrollee Ratio. The minimum proportion of the number of providers of a given type per enrollee.
- Appointment waiting time. Set maximum wait times for patients to receive care (urgent and non-urgent cases).
- accept new patients. Determine the minimum number or percentage of providers willing to accept new patients.
State Medicaid agencies must specify network adequacy standards and enforce them for any Medicaid Managed Care Organization (MCO). Affordable Care Act (ACA)
The first national standard for network adequacy was developed, but only for Qualified Health Plans (QHPs) in the commercial insurance marketplace sold through the health insurance exchange marketplace. The RWJF briefing notes that these standards are often very different. The Medicaid MCO allows enrollees to drop out of the plan if the network is imperfect, has quantified entry criteria, and needs to be enforced by the state; the ACA QHP requires none of these things to happen.
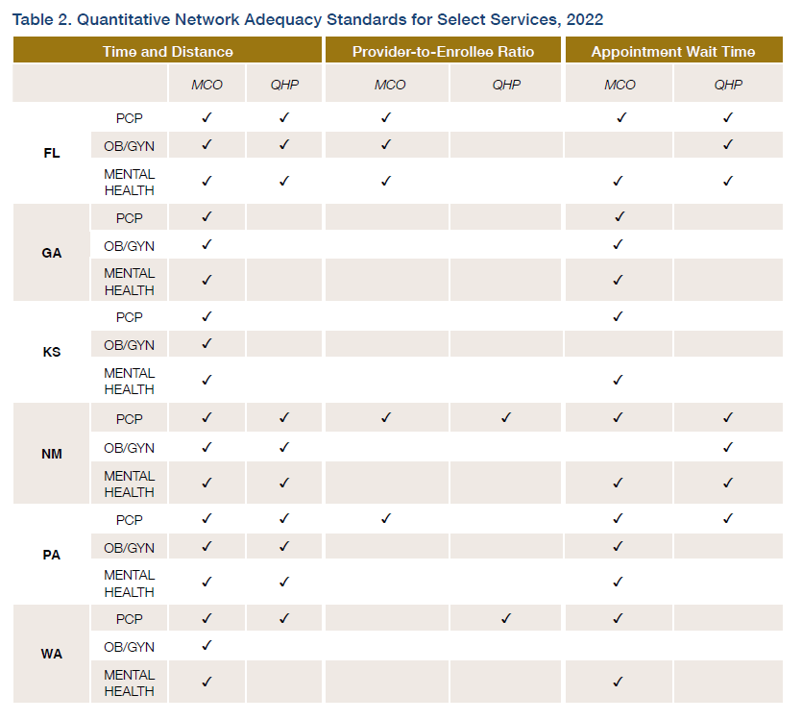
Additionally, different states have different network adequacy standards for different providers. In this study, the authors reviewed federal laws, regulations, and sub-regulatory guidelines for the MCO and QHP programs. The table below provides and summarizes their conclusions from the 6 state case studies.
The recommendations in the report are largely based on more regulation: (i) more oversight, (ii) more consumer protection, (iii) more transparency, and (iv) more enforcement. However, the effectiveness of these enforcement mechanisms is unclear. Greater transparency and standardized reporting would help so that Medicaid MCO beneficiaries and commercial QHP participants can better showcase different plan offerings.
[ad_2]
Source link








